Turning our Thoughts to our Hearts
It’s February. Our thoughts turn to matters of the heart. First, it’s American Heart Month, a time to spotlight heart disease, a leading cause of death in the United States and the world. This year marks the 57th anniversary of American Heart Month. In 1964, President Lyndon B. Johnson, a heart attack survivor himself, issued the first proclamation to increase awareness about heart disease and it continues today.
Wear Red This Friday
The first Friday of American Heart Month, Feb. 5, is National Wear Red Day, focusing on the issue of heart disease in women. Did you know that 1 out of 3 women are diagnosed with heart disease each year? Too many. On Friday, Feb. 5th, across the country, billboards, buildings, and millions of people will go red in support of the fight against heart disease. For more information on joining the campaign, visit goredforwomen.org.
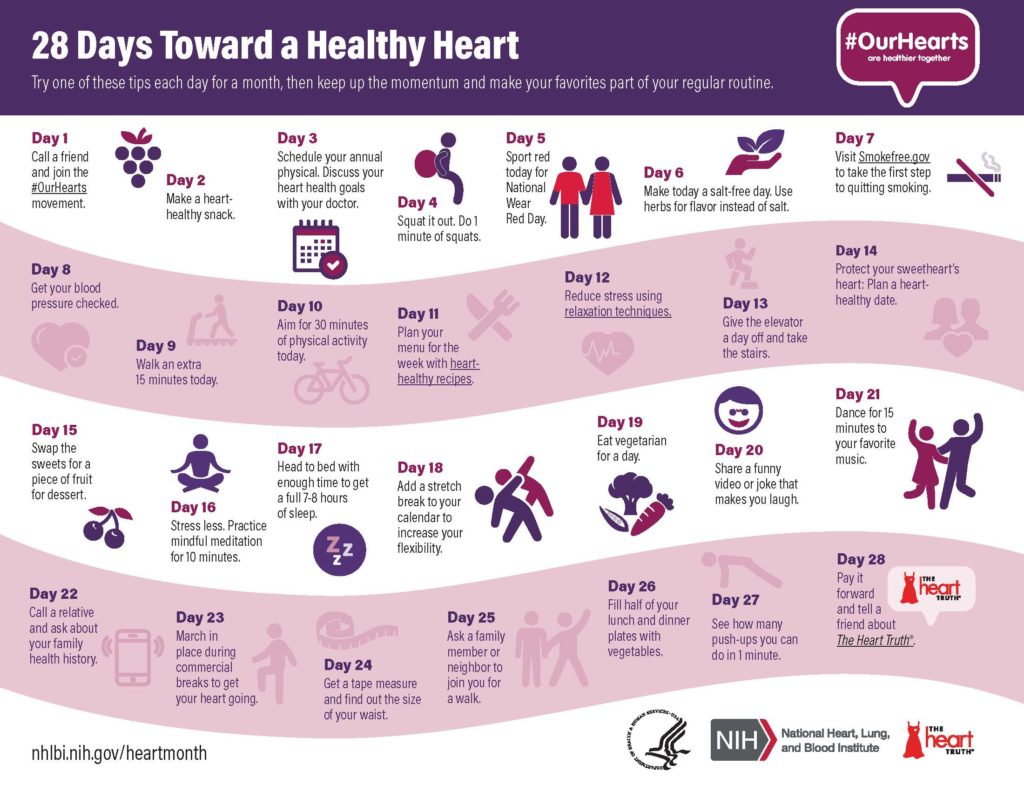
A Healthy Heart
Furthermore, this year American Heart Month is more important than ever due to the impact of the COVID-19 pandemic. For example, research on the coronavirus suggests that it has potential harmful effects on the heart and vascular system. Additionally, more people have delayed or avoided going to the hospital when they had symptoms of a heart attack, resulting in more deaths from heart disease. Then, there is the issue of living in lockdown – eating more, drinking more alcohol, and exercising less, all of which contribute to heart disease.
It’s important to take steps that help heart health, especially since heart disease continues to be a leading cause of death in not only the U.S., but across the globe. In 2019, more than 18 million people in the world died of heart disease, an increase from the previous decade. There is more work to do in this area to ensure that we live longer and healthier.
Heart Month and Valentine’s Day
During February our thoughts also turn to love as we celebrate Valentine’s Day. If you think about it, these two events, American Heart Month and Valentine’s Day, are related. They are both about love.
According to the Ancient Greeks, there are six types of love:
- Eros, named after the Greek god of fertility, involves passionate love and loss of control, e.g., falling madly in love;
- Philia involves deep comradery and loyalty — your BFFs; another kind of Philia called Storge represents love for your family
- Ludus is teasing, playful love, aka flirting
- Agape is selfless love and is the origin of the word “charity”
- Pragma is described as mature, realistic love; standing in love – making an effort to give love rather than receive it – think long term relationships.
- Philautia is self-love; too much leads to narcissism and obsession, but the idea is to like yourself and feel secure in yourself so that you have love to give others.
I believe the message from the Greeks is that we should nurture the many varieties of love. Don’t just seek eros, cultivate philia by spending more time with old friends, or develop ludus by dancing the night away. The beauty of this is we can do this today even during the pandemic. Simple acts of love can go a long way to help others who are weary and weathered from the struggles of this past year.
And then there’s philautia, self-love. We owe it to ourselves to have a healthy heart. We foster this by adopting the following: a healthy lifestyle, including not smoking, maintaining a healthy weight, controlling blood sugar and cholesterol, treating high blood pressure, getting at least 150 minutes of moderate-intensity physical activity each week, and getting regular checkups.
There is still time to make positive changes for 2021. Love your heart. Love yourself. Love others. Be loved.
Author: Tracy Chamblee, PHD, APRN, PCNS-BC, CPHQ, CPPS
Clinical Executive