National Nurses Week 2022
National Nurses Week is dedicated to celebrating the amazing, challenging, and sometimes heart-breaking contributions nurses make to the medical world. Nurses are pinnacle to delivering medical care, from assisting with delivering babies to life-threatening emergency room crises to ensuring that every patient receives the direct and proper care they need. National Nurses Week starts each year on May 6 and ends on May 12, which is Florence Nightingale’s birthday.
Today, professional nurses work in a variety of healthcare settings such as hospitals, doctor’s offices, Academic Medical Centers, and community organizations. National Nurses Week celebrates the hard work nurses endure every day as they care for their patients. This month’s theme is “Nurses Make a Difference.”
Nurses make a difference as trusted advocates of patients. Nurses make a difference by helping to shape medical care. Nurses make a difference by educating, innovating, and advocating for the health and well-being of their communities.
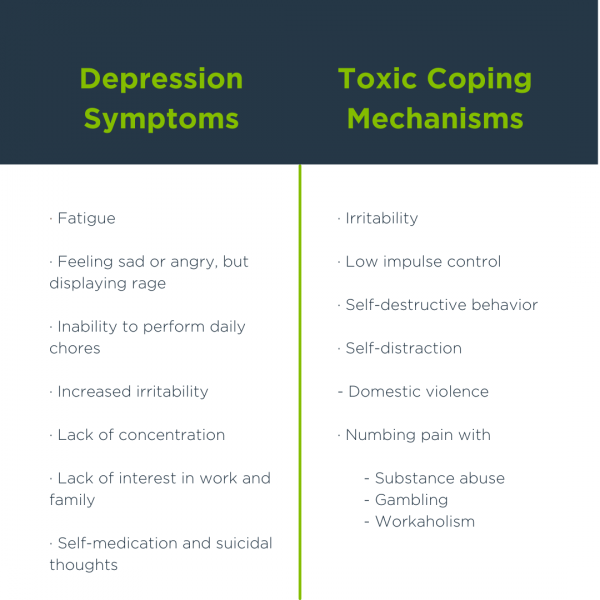
Becoming a nurse requires four years of study, hard work, and dedication. However, burnout in this profession is a real issue characterized by mental, emotional, and physical exhaustion. Some of the reasons for burnout include long work hours, staff shortages, and a stressful work environment. Nurses have sacrificed so much, especially during the pandemic.
Celebrating National Nurses Week allows the community to understand and appreciate the incredible work nurses do. They are an essential part of the medical world. This is why, during National Nurses Week, SaferCare Texas chooses to recognize nurses worldwide for their incredible work in their community.
Throughout the week, SaferCare Texas celebrates nurses through:
- May 6, National Nurses Day: Join SaferCare Texas live on Facebook @2pm as Director John Sims speaks about just culture
- May 10: SaferCare Texas will be releasing a video of our nurses as they answer questions about their professional experience and their assessment of where the profession is going
- May 11, National School Nurse Day: SaferCare Texas will be introducing a brand-new initiative to celebrate health heroes in our community. Asthma411 Health Heroes is a collaboration between SaferCare Texas, Cook Children’s, and JPS Acclaim.