It’s been a little over 2 months since I joined the HSC and SaferCare Texas family. Wow. Time flies, even during a pandemic. In my new role, I learn something new every day. One of my passions is healthcare quality. Yes. You read correctly. I love all things quality and safety.
This week is National Healthcare Quality week. In recognition of this week, the focus of this blog is on quality. The term quality is often a catchall term. According to Merriam-Webster, definitions of quality include how good or bad something is, a characteristic or feature, high level of value or excellence, and the standard of something as measured against other things of a similar kind.
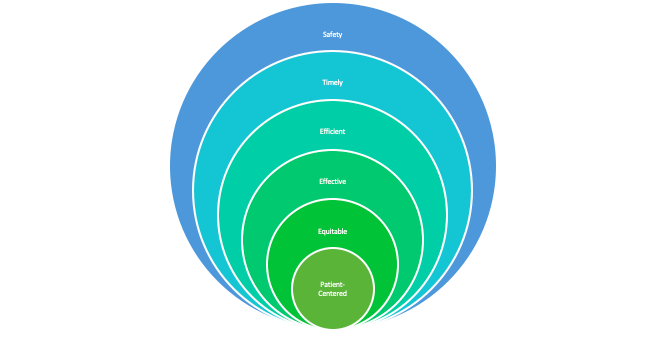
In healthcare, when we speak of quality it typically has multiple meanings depending on one’s viewpoint. My favorite definition of quality is the one that is put forth by the National Academy of Medicine, formerly the Institute of Medicine. Quality is care that is SAFE, TIMELY, EFFECTIVE, EFFICIENT, EQUITABLE and PATIENT-CENTERED (STEEEP). In this definition, safety serves as the foundation of quality. In short, quality does not exist without safety.
The Quality Model
Let’s go a little deeper into this. Did you know that a healthcare organization’s culture impacts the quality of care provided?
At SaferCare Texas, one of our priorities is providing education to help others make the connection between culture and safety. An organization’s culture is comprised of the collective beliefs, attitudes, perceptions, and values of its leaders and employees. This includes the beliefs, attitudes, perceptions, and values regarding safety. How would you describe your organization’s culture? Did you know that you can measure it?
Measuring Safety Culture
There are many safety culture surveys available for use. But the one that most people are familiar with is the Survey on Patient Safety (SOPS) developed by the Agency for Healthcare Research and Quality (AHRQ). This survey was originally designed for use in hospitals but has been modified for use in other healthcare settings such as primary care. The survey helps healthcare organizations assess safety culture within their own walls.
Who takes the survey?
All team members across the organization – providers, nurses, technicians, non-clinical staff, etc. participate. It is a tool to help an organization assess its safety culture strengths and weaknesses. This survey is not a one-and-done survey. In fact, most healthcare organizations ask team members to complete the survey every 12-24 months. By doing so, organizations can re-assess their safety culture, and determine which improvement interventions were successful, and what opportunities remain. Remember, improving safety culture takes years sometimes.
The survey results help identify local or system level quality improvement projects such as improving patient handoffs or improving communication between healthcare providers. These are just a few reasons why regularly assessing culture should be the norm.
Example of Safety Culture
Let me share an example of safety culture from a different healthcare setting. Medical Transport. Specifically, flight transport. Several years ago, a colleague of mine worked as a flight nurse. I was amazed to hear her share stories of safety time-outs that were done if someone on the team felt something was not quite right or referring a case to another agency due to team exhaustion. It was obvious that the culture of safety was more advanced in this setting. Later on, I learned that this was due to the connection of the air-based transport team with aviation. Today, more than a decade later, safety precautions like time-outs, are commonly practiced in many healthcare settings.
How to Approach Errors
If you are a leader, do you think your team members feel empowered to come to you with concerns about an unsafe situation or when a mistake occurs? Have you empowered your team to speak up without the fear of repercussions from their colleagues or administration?
How the organization approaches errors is another aspect of organizational culture. Healthcare has a long tradition of holding individuals accountable for errors or mishaps that happen to patients under their care. Let’s face it – people are fallible. People make mistakes. Mistakes can contribute to harm to a patient or another team member. However, punishing an individual for a mistake does not solve the problem. One of my favorite quotes on this topic is this:
The single greatest impediment to error prevention in the medical industry is “that we punish people for making mistakes.”Dr. Lucian Leape, Harvard School of Public Health
Just or Fair Culture.
In healthcare, people function within systems and use processes designed and put into place by the organization. A person may make a mistake, but the system or process that they were following is also an issue. The reality is — there is no such thing as a perfect system, a perfect process, or a perfect human. Perfection does not exist. So, when we punish a person for making a mistake and we fail to address the system or process issue, the problem goes unchecked and patients or team members will continue to suffer harm.
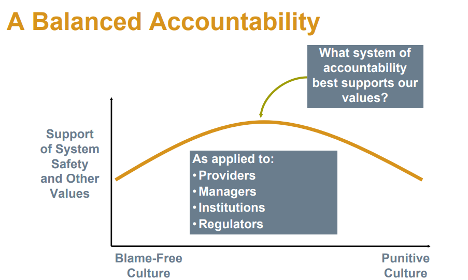
To address this, organizational leaders must shift the focus from errors and outcomes to system design and management of the behavioral choices of team members. This shift is known as Just or Fair Culture. Yes. Another aspect of organizational culture. The concept of Just or Fair Culture is related to systems thinking which emphasizes that mistakes are generally a product of faulty organizational cultures, rather than solely due to the person or persons directly involved.
Consider the following situation:
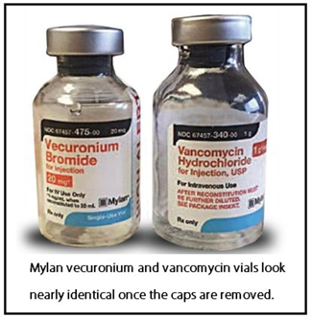
A nurse working in a busy clinic inadvertently takes the wrong vial of intravenous medication from the dispensing system and administers the drug to a patient. Subsequently, the patient experiences a cardiac arrest. What is the best way to approach the nurse and investigate the situation?
The investigation revealed that 2 vials of entirely different medications looked alike in shape, size, color, and print and were located right next to each other in the medication dispensing system. This is an accident waiting to happen and it did. Human error was involved, but the nurse should be consoled and supported by her leader rather than punished. Think about it. In this scenario, the system of medication storage is faulty and in need of improvement. Working within this system, the nurse was set up to fail. The fix for this issue is improving medication storage.
A just culture creates balanced accountability. Creating the need for open and honest reporting with the end goal of cultivating a culture that is focused on continuous learning. See the image below for a visual.
For more information on Just Culture, please see https://www.justculture.com.
Finally, did you know that the concept of safety culture originated outside healthcare? Industries such as aviation and nuclear power plants are known as high reliability organizations (HROs) because they consistently minimize adverse events despite carrying out complex and hazardous work. HROs maintain a commitment to safety at all levels, from frontline providers to managers and executives. This commitment establishes a culture of safety. Key features of HROs include:
When you think about it, quality is everyone’s responsibility every day. Quality in healthcare means providing the care the patient needs when the patient needs it, in an affordable, safe, effective manner.
I encourage you to take some time this week to recognize someone you work with for their efforts to ensure patients receive safe, timely, efficient, effective, equitable and patient-centered care.
For more information on healthcare quality, register for our upcoming panel discussion on improving healthcare quality through leadership education and making the case for quality and safety embedded in academic programs.
Author: Tracy Chamblee, PHD, APRN, PCNS-BC, CPHQ, CPPS
Clinical Executive at saferCare Texas