Health Worker Safety: A Priority for Patient Safety

Patient Safety is a global priority. In recognition of this, the World Health Organization (WHO) established World Patient Safety Day in May 2019 as an annual event. The objectives of this initiative are: 1) increase public awareness and engagement, 2) enhance global understanding, and 3) spur global solidarity and action to promote patient safety.
The origin of this day is firmly grounded in the fundamental principle of medicine – First, do no harm.
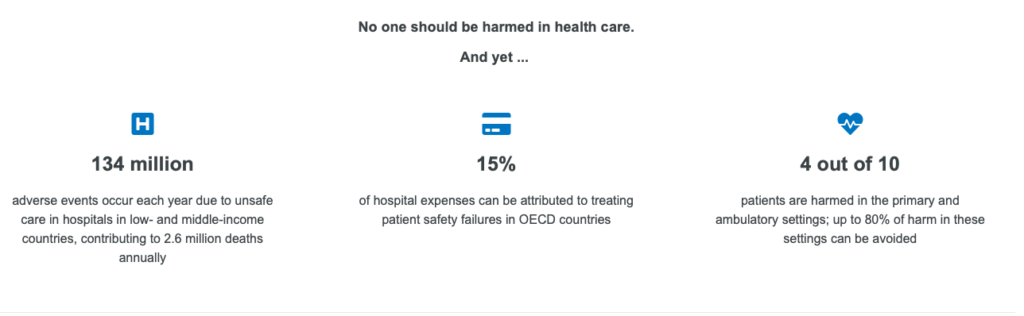
Patient Safety is a relatively young discipline that emerged on the heels of the Institute of Medicine (IOM) report, To Err is Human, which reported 44-98,000 deaths per year were attributed to medical error — adverse events. Initially, this work was focused on care in the hospital setting. Twenty years later, we now recognize that harm occurs in ALL health care settings, and we also know that most of the harm associated with adverse events is preventable.
It is also reported in the literature, that medical errors in the U.S. are considered the 3rd leading cause of death at 440,000 per year, behind heart disease and cancer.
Since these reports, we have made great strides to improve patient safety in the U.S., but we still have opportunities to improve. The focus on patient safety is moving into other health care settings like ambulatory care. This is the new face of patient safety.
This year, the COVID-19 pandemic has brought to light existing issues among health care professionals related to burnout and mental health issues, such as depression and anxiety. This is a global problem. Issues such as health care associated infections, workplace violence, bullying and harassment, stigma, psychological and emotional disturbances, illness, and even death. Working in a stressful environment increases the likelihood of errors which can lead to patient harm or harm to a fellow team member.
At SaferCare Texas, our mission is to eliminate preventable harm. We do this through education, advocacy, and by challenging traditional thinking as it relates to quality and safety in any health care setting. This year we want to join World Patient Safety Day 2020 and bring awareness to health care worker safety. This year’s theme is:
Health Worker Safety: A Priority for Patient Safety
You might be thinking, how does health care worker safety impact patient safety? The truth is if health care workers do not feel safe in their work environment, how can we expect them to keep patients safe.
Going back a little further, let’s define safety. In my humble opinion, the best definition of safety is: a dynamic non-event. Think about it. In order to keep everyone safe, the organizational culture must prioritize safety in the workplace. To do this, leaders must set the tone and role model that everyone safe is a priority. Safety is the foundation of the organizational culture.
This year’s World Patient Safety Day slogan is: Safe healthcare workers, Safe patients. It is very timely. Health care has a long history of being a stressful environment. I have worked in health care for more than 30 years and have experienced it first-hand. Let’s face it – we are all humans. We are fallible, and we make mistakes. However, working in a stressful environment increases the likelihood of errors that can result in harm to a patient or a team member.
The ongoing experience of health care workers across the globe during this pandemic is a great example – lack of personal protective equipment (PPE). Imagine working in an environment and not feeling safe. This is a real issue impacting health care workers every day and can lead to mental health issues such as depression, anxiety, even suicide. It’s a real problem. We need to empower health care workers to speak up and voice their concerns about working conditions.
Another important workplace issue is violence, physical assault by patients, caregivers or even team members as well as verbal abuse, harassment, and bullying. Yes, this happens often in health care and is not acceptable. Workplace violence also contributes to the mental health issues described above.
Globally, an estimated 264 million people suffer from depression. Depression is one of the leading causes of disability. And many people who suffer from depression also suffer with symptoms of anxiety. Mental health issues such as this have a significant economic impact related to lost productivity. The global estimated cost is $1 trillion/year. And, in many cases, these issues are preventable.
This is why psychological safety is so important. If you are not familiar with the term, psychological safety in the workplace is the belief that you won’t be punished when you make a mistake. Yes, when you make a mistake. Acknowledging your humanness is the first step. Because psychological safety in the workplace is so important, the WHO also issued the following Call to Action:
Speak Up for Healthcare Worker Safety
At SaferCare Texas, we challenge you to be empowered and to empower your colleagues to speak up, let someone know if you do not feel safe in your work environment. In addition to this, the Institute for Healthcare Improvement (IHI) recently launched a campaign on psychological safety called “Your Psychological Personal Protective Equipment (PPE). This campaign outlines strategies that both individuals and leaders can do to promote mental health and wellbeing.
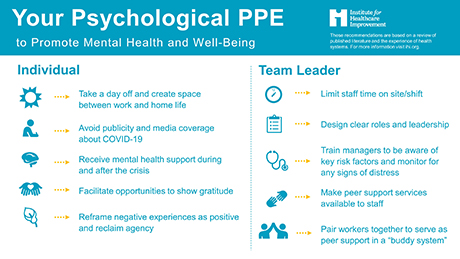
You can find more information about IHI’s psychological safety campaign here.
Author: Tracy Chamblee, PHD, APRN, PCNS-BC, CPHQ, CPPS – Clinical Executive at SaferCare Texas