Geriatrics and Patient Safety
By Dr. Kate Taylor, DNP, FNP-C, CPPS, FNAP
According to Uptodate.com, a widely used resource for healthcare professionals, 90,000 older adults die in the US as a result of injury. If you look up injuries and older adults on the general web, you find a lot of information about falls. Falls account for over half of the injuries of older adults. The Centers for Disease Control provides great detail about fall prevention. In this blog, you will get a few take-home tips addressing home safety with older adults.
Why do older adults get injured? Older adults have injuries due to physical disability, cognitive impairment, and increased risk of isolation or problems with communication. Older adults also depend more on others for everyday living activities, which puts them at higher risk for injury.
The finances of older adults continue to be affected. The poverty rate is declining over the past 50 years, but 10% of the elderly population still live at or below the poverty line. Blacks and Hispanics have a higher rate of poverty. Your healthcare provider needs to screen older adults with financial and social resources as it directly impacts health status and well-being.
Lastly, social isolation affects patient safety in the home as well. Older adults have increased social isolation due to functional limitations, and a lack of relatives, friends, or organizations. This can mean that older adults experience higher rates of depression, anxiety, disability, and self-rated poor health. Again, your healthcare provider needs to screen for these things.
There are abundant preventable home safety concerns. Let’s tackle a few of them today.
Each year, more than 90% of exposures reported to the local poison control centers occur in the home!
Be prepared: Have a number available for text 797979
- Practice safe storage habits: Medications, cleaning supplies, pesticides, button batteries, oils (such as tiki torch oil), personal care products, and chemicals
- Read and follow labels and directions
- Prepare food safely: Prepare, cook, and store
Choking is a big safety concern!
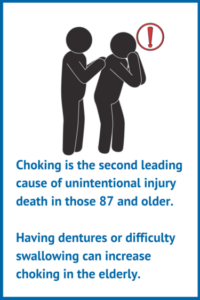
- Eat foods with minimal choking risk such as ground meat, soup, Jello, applesauce, fish, and chocolate
- Avoid foods with high choking risk such as steak, hard candy, popcorn, white bread, hot dogs, cake and milk, dry crackers, and chicken with bones
Carbon monoxide poisoning harms!
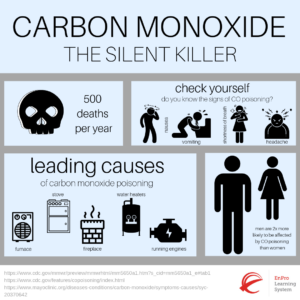
- Never try to heat your home with your stove, oven, or grill since these can give off carbon monoxide.
- Make sure there is a carbon monoxide detector near all bedrooms, and be sure to test and replace the battery twice a year.
Elder abuse is sad but true and occurs in 1 in 10 adults over the age of 60.

There are many types of abuse of older adults, but the most common is financial abuse that can occur from the following:
- Financial neglect: The older adult’s bills such as utility, personal, or property taxes are not getting paid.
- Financial exploitation: Misuse of finances by the use of intimidation or manipulation or without consent.
- Healthcare fraud: The healthcare team charges too much, falsifies claims, or charges for care but does not provide the healthcare service.
Call the police or 911 if someone is in immediate, life-threatening danger or use the Eldercare Locator.

The evidence is not robust on how to avoid home-based older adult injuries, except for those recommendations provided by the CDC on fall prevention. In my opinion, the best geriatric safety prevention plan is the Medicare Annual Wellness Visit (AWV). This is a paid visit covered by Medicare part B. Your provider will ask questions and conduct screening questionnaires, which in turn, provide you with a personalized health plan based on your health and risk factors.
Additional Resources:
- HealthinAging.org and their home safety tips for older adults
- National Center on Elder Abuse handout on Red Flags of Abuse
- National Institute of Aging and good checklist on home safety checklist for Alzheimer’s Disease
References:
Uptodate.com
CDC (Center for Disease Control, www.cdc.gov)
NIH (National Institutes of Health, www.nih.gov)
Poison Control (poison.org)
Medicare.gov



