To Lose A Son: A Father’s Despair
Author: John Sims, MSN, RN, CNL – Director of SaferCare Texas
Today, September 10, marks Global Suicide Prevention Day, with the month of September being recognized as National Suicide Prevention Month. For some people it’s just another awareness day on the calendar, but for me it hits closer to home.

Clay’s Story
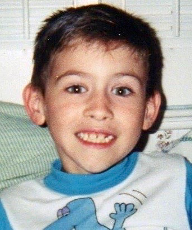
Three years ago, I lost my beautiful son to suicide.
John Clayton Sims, named after my paternal grandfather, was my oldest son and a great man. As a child, Clay was well behaved even with his struggle in school due to a dysgraphia diagnosis. This led to my wife and I’s decision to hold him back in third grade. Unfortunately, his classmates quickly noticed his third-grade retention and immediately poked fun at him, igniting extreme sadness.
His behavior slowly started to change when he entered his teenage years. He became more aggressive and started drinking excessively. I rationalized these behaviors as hard adolescent challenges but felt powerless to change them.
After the 9/11 terrorist attacks, Clay made a commitment to serve his country and join the Army. I was a proud father. After basic training, my family and I went to visit him and were greeted by a new Clay. His glowing, confident appearance was something I had not seen in quite some time. He seemed to have found a new life purpose.
Sadly, he sustained a knee injury during a 16-mile ruck march and was honorably discharged. He returned home and shortly thereafter began to experience several mental health issues. While in intense, outpatient-alcohol treatment, the psychiatrist suspected bipolar disorder, and recommended long-term inpatient treatment for confirmation. His long-term therapy abruptly ended despite insurance appeals. Following his pre-mature discharge from treatment, Clay transitioned to sober houses with strict guidelines; he had to take his meds (for his bipolar disorder) and attend meetings. Clay resided in two sober houses before leaving on his own will after 7 months.
Not long after, we received that dreaded knock on the door that our beautiful 23-year-old son had taken his own life. My worst nightmare had come true, leaving a permanent hole in my heart.
I, among many others in my family, have been left trying to navigate the devastating grief and unanswered questions. We torment ourselves wondering if we did enough, did we do too much, what if we had tried this, or that, and so on. We have found ourselves in the endless circle of “what-ifs.”
Thankfully, we have had a great support system. Our church friends and family responded by providing emotional support, meals, and housecleaning. We joined a local bereavement support group “Survivors of Suicide”, an excellent vehicle for shared, painful emotions. The rawness of this group proved too painful for my grief, so we transitioned to an eight week Trauma Grief Class. Eye Movement Desensitization and Reprocessing (EMDR) therapy also helped us minimize the intense emotion associated with our son’s death.
Three years later, we still attend family counseling around this topic. Thus far, we have been unable to find closure, but do find temporary peace sharing his story, hoping it opens a dialogue for those in similar circumstances.
Suicide Prevention
With suicide rates rising, I felt compelled to share Clay’s story and hope to bring awareness and prevention measures to those in need.
Sadly, suicide ranked 10th in leading causes of death overall in the U.S. in 2017, claiming more than 47,000 lives, and 800,000+ globally according to the CDC. Over 121 individuals’ complete suicide on a daily basis.
Additionally, the environment we are living in today due to Covid-19 has elevated levels of adverse mental health conditions, substance use, and suicidal ideation. According to a recent CDC study, mental health conditions are disproportionately affecting specific populations, especially young adults, Hispanic persons, black persons, essential workers, unpaid caregivers for adults, and those receiving treatment for preexisting psychiatric conditions.
It’s crucial that we pay attention to warning signs and reach out when we think someone is in need. Below I have compiled a list of suicide awareness resources for you to use to help prevent this health crisis.
· National Suicide Prevention Lifeline – can all help prevent suicide. The Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals. 1-800-273-8255
· American Association of Suicidology is an association for mental health and public health professionals, researchers, suicide prevention and crisis intervention centers, school districts, crisis center volunteers, survivors of suicide loss, attempt survivors, and…
· Crisis Text Line Text HOME to 741741 from anywhere in the United States, anytime. Crisis Text Line is here for any crisis. A live, trained Crisis Counselor receives the text and responds, all from our secure online platform. The volunteer Crisis Counselor will help you move from a hot moment to a cool moment.
· The Dougy Center – The National Center for Grieving Children and Families provide support in a safe place where children, teens, young adults and their families grieving a death can share their experiences.
· How to Talk to a Child about a Suicide Attempt in Your Family (Rocky Mountain MIRECC) This guide is intended to provide you with some of that support, and also share other resources that may be helpful for you now and as your family recovers.
· The Jason Foundation – The Jason Foundation, Inc. (JFI) is dedicated to the prevention of the “Silent Epidemic” of youth suicide through educational and awareness programs that equip young people, educators/youth workers and parents with the tools and resources to help identify and assist at-risk youth.
· The Jed Foundation empowers teens and young adults with the skills and support to grow into healthy, thriving adults
· Lifeline Chat is a service of the National Suicide Prevention Lifeline, connecting individuals with counselors for emotional support and other services via web chat. All chat centers in the Lifeline network are accredited by CONTACT USA. Lifeline Chat is available 24/7 across the U.S.
· Man Therapy gives men a resource they desperately need. A resource to help them with any problem that life sends their way, something to set them straight on the realities of suicide and mental health, and in the end, a tool to help put a stop to the suicide deaths of so many of our men.
· Mental Health America is the nation’s leading community-based nonprofit dedicated to addressing the needs of those living with mental illness and promoting the overall mental health of all.
· My3 App lets you stay connected when you are having thoughts on suicide.
· National Action Alliance for Suicide Prevention is the nation’s public-private partnership for suicide prevention. Current priority areas include: transforming health systems, transforming communities, and changing the conversation.
· National Organization for People of Color Against Suicide primary focus and mission is to increase suicide education and awareness. We offer unique opportunities for outreach partnerships and community education efforts directed at communities of colors across the nation.
· Now Matters Now teaches Mindfulness, Mindfulness of Current Emotion, Opposite Action and Paced breathing. These skills are part of Dialectical Behavior Therapy or DBT, proven to be helpful for people considering suicide.
· Parents, Families, Friends, and Allies United with LGBTQ People (PFLAG) mission is to build on a foundation of loving families united with LGBTQ people and allies who support one another, and to educate ourselves and our communities to speak up as advocates until all hearts and minds respect, value and affirm LGBTQ people.
· Safety Planning Tools is a written, prioritized list of coping strategies and resources for reducing suicide risk. It is a prevention tool that is designed to help those who struggle with their suicidal thoughts and urges to survive.
· SAVE was one of the nation’s first organizations dedicated to the prevention of suicide. Our work is based on the foundation and belief that suicide is preventable and everyone has a role to play in preventing suicide. Through raising public awareness, educating communities, and equipping every person with the right tools, we know we can SAVE lives.
· The Society for the Prevention of Teen Suicide mission is to reduce the number of youth suicides and attempted suicides by encouraging public awareness through the development and promotion of educational training programs.
· StopBullying.gov provides information from various government agencies on what bullying is, what cyberbullying is, who is at risk, and how you can prevent and respond to bullying.
· Suicide Prevention Resource Center is the only federally supported resource center devoted to advancing the implementation of the National Strategy for Suicide Prevention. SPRC is funded by the U.S. Department of Health and Human Services’ Substance Abuse and Mental Health Services Administration (SAMHSA) under grant no. 5U79SM062297 and is located at Education Development Center.
· Teen’s Health gives you the tools and confidence to make the best health choices. TeensHealth.org is part of the KidsHealth website.
· The Trevor Project is the leading national organization providing crisis intervention and suicide prevention services to lesbian, gay, bisexual, transgender, queer & questioning (LGBTQ) young people under 25.
· Emdria.org a resource for learning more about EMDR therapy and to locate an EMDR therapist in your area
· Veterans Crisis Line – If you’re a Veteran in crisis or Service member in crisis — or you’re concerned about one — there are caring, qualified VA responders standing by to help 24 hours a day, 7 days a week.
· Wounded Warrior Project is committed to helping those living with PTSD




