COPD and Covid-19: What to Know
The pandemic has changed our way of life, and forced us to establish a new “normal.” There is much dialogue around chronic health conditions at risk for severe illness from Covid-19. Most discussions emphasize diabetes, obesity, and auto-immune disorders, but few mention chronic obstructive pulmonary disease (COPD).
COPD refers to a group of diseases that cause airflow blockage and breathing-related problems. It includes emphysema and chronic bronchitis1. COPD causes airway inflammation, increased mucous production, and weakening of the parts of lungs where gas is exchanged2. We breathe in oxygen and breathe out carbon dioxide. In people with COPD, this process is impaired, producing lower than normal oxygen levels, and higher than normal carbon dioxide levels. As the disease progresses, this results in low energy and somnolence.
What Causes COPD?
Air pollutants in the home and workplace, genetic factors and respiratory infections play a role. The most common air pollutant is tobacco smoke-both first and second hand. People should avoid smoking tobacco or inhaling others’ smoke. Also, ensure proper ventilation in indoor spaces. Early COPD detection may slow disease progression.3
According to the CDC, 140,000 Americans die each year from COPD and 75% of those deaths are attributed to smoking. It is estimated that 15 million currently have COPD, and as many as 12 million have yet to be diagnosed4.
COPD Symptoms
Diagnosing COPD can be done in your doctor’s office with a special breathing apparatus called a spirometer. Please contact your doctor if you have experienced any of the following symptoms:
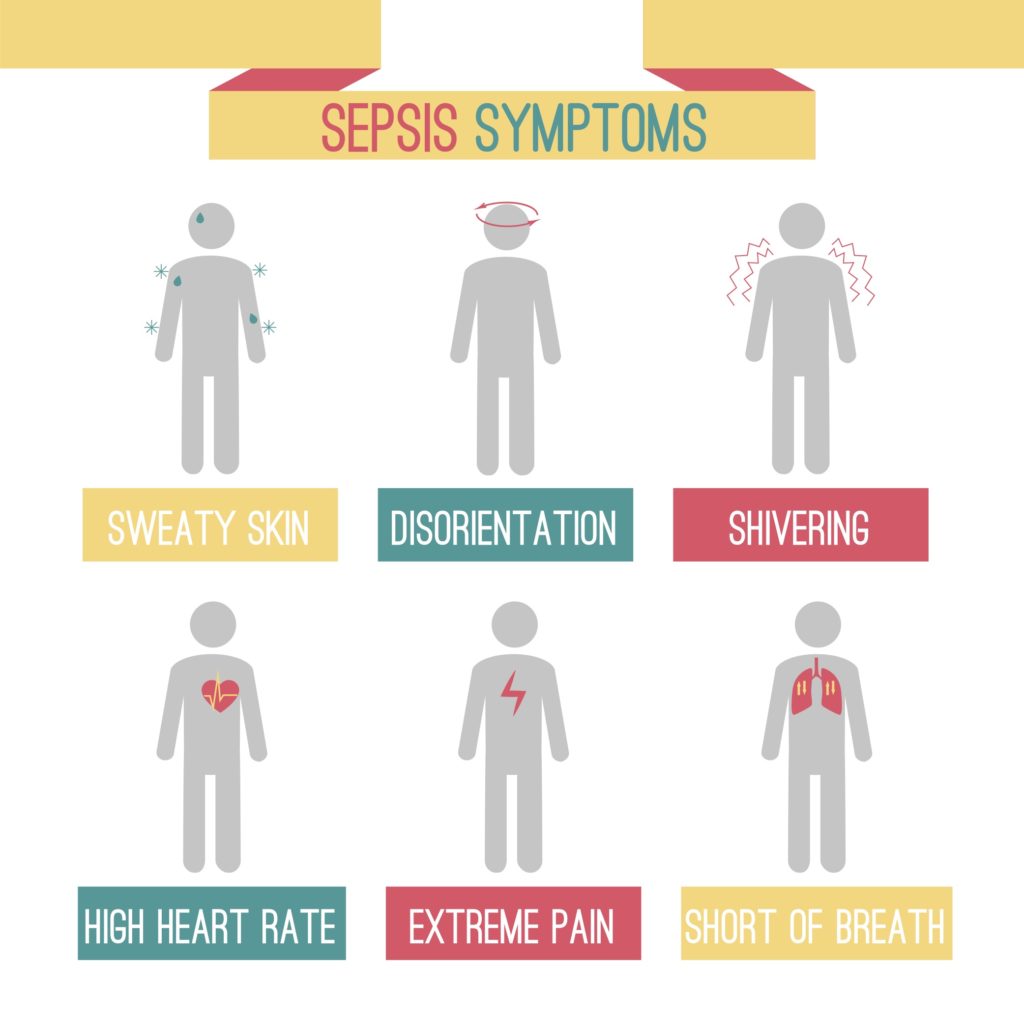
Commonly, people with COPD contract pneumonia and other respiratory infections, leading to frequent hospitalizations. These infections cause an increase in the severity of COPD, referred to as a COPD exacerbation. As the symptoms intensify, patients become less tolerant to activity; simple tasks such as walking to the bathroom, tying shoes, and in severe cases, eating expend so much energy that rest periods are necessary. The combination of symptoms can cause dizziness, lethargy, frequent shortness of breath, and others.
Treatment for COPD exacerbations requiring hospitalizations include antibiotics for the infection, nebulized breathing treatments, and steroids. Steroids and breathing treatments reduce inflammation; however, steroids also reduce the body’s immune response to infection. This vicious cycle ends in death as noted earlier.
How can people with COPD stay safe during the Pandemic?
People with COPD are at increased risk for severe illness from Covid-19. Both ailments affect the respiratory system. People with COPD have chronic difficulty breathing, and therefore should refrain from wearing masks, as per CDC guidelines5.
To sustain optimal health with COPD, during the pandemic, please follow this advice5:
- Stay at home as much as possible. Look into delivery services, or enlist a trusted family member.
- Avoid sick people
- Keep your hands clean
- Avoid touching your face, especially with unclean hands
- Disinfect frequently used surfaces/objects
- Reduce stress-contact family members via phone/virtual platforms
- Continue your COPD maintenance plan as prescribed by your doctor
- Make sure you maintain a supply of your prescribed medications
- Telemedicine is an innovative way to see your doctor; call if your symptoms begin to worsen
- Avoid COPD exacerbation triggers such as smoking/vaping or other environmental pollutants
References
1. Aryal, S., Diaz-Guzman, E., & Mannino, D. M. (2014). Influence of sex on chronic obstructive pulmonary disease risk and treatment outcomes. International journal of chronic obstructive pulmonary disease, 9, 1145–1154. https://doi.org/10.2147/COPD.S54476
2. Centers for Disease Control and Prevention. Annual smoking-attributable mortality, years of potential life lost, and productivity losses — United States, 1997–2001. MMWR Morb Mortal Wkly Rep. 2005;54(250):625–628.
3. Centers for Disease Control and Prevention. National Vital Statistics System detailed mortality data at Wonder Database website. http://wonder.cdc.gov. Accessed July 3, 2019.
4. Centers for disease control. (2020, February 20). World Life Expectancy. Retrieved November 19, 2020, from https://www.worldlifeexpectancy.com/usa-cause-of-death-by-age-and-gender
5. National Center for Immunization and Respiratory Diseases (NCIRD) Division of Diseases. (2020, November 12).