Healthy Food Plants the Seed for Health Equity

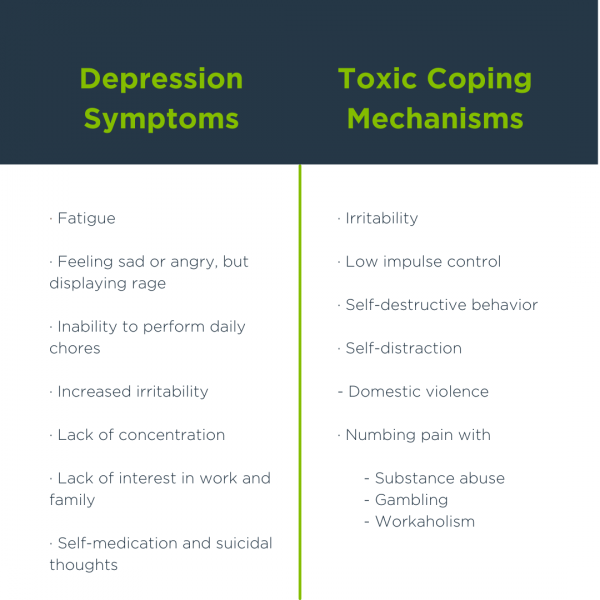
People who live in food deserts that have low income and no transportation are particularly affected by numerous social determinant barriers to good health.1 Children who grow up eating unhealthy food may experience long-term impact on their food preferences and health later in life.2 Limited opportunity to learn good health practices – low health literacy – perpetuates poor health and poverty causing a vicious cycle that starts with each generation of children. In fact, food insecurity is linked to health disparities in children including:
- Fair or poor health,
- Iron deficiency,
- Lower cognitive performance,
- Behavioral issues,
- Parental mental health issues,
- Asthma,
- Depression, anxiety & suicidal thoughts and
- Poor dental health.3
For all populations, good health and nutrition are important for prevention and management of chronic conditions such as obesity, heart disease, diabetes, and some types of cancer. Proper nutrition is one aspect of preventing obesity, which is a major health risk globally and in the United States.4 While the importance of good nutrition is well understood by healthcare providers, putting nutrition recommendations into practice can be difficult for many families challenged by food insecurity and low health literacy.
When we consider Maslow’s hierarchy of needs, it becomes clear that meeting basic physiological needs such as hunger can help communities progress towards health equity by reaching higher hierarchal levels of social and civic activities needed to change social infrastructure. These changes are important to the equitable future of children as healthy lifestyles and disease prevention should start early in life.
Improving health literacy among other social determinants of health can help with resolving health disparities such as observed with Covid-19.5 To decrease health disparities and thus, impact health equity, focus placed on resolutions to social determinant issues will plant the seeds that grow into an equitable future:
- Multi-faceted interventions to address social infrastructure;
- Increased self-efficacy by empowering people to navigate the current healthcare system and make healthy decisions; and
- Health and nutrition literacy policy strategies to overcome the complex phenomena of social determinants and empower people to eat healthy and reduce disease risk among populations.1
The seeds that resolve food insecurity can also resolve health disparities nourishing equal health opportunities for all communities and combatting future public health disparities experienced in Covid-19.5
Author: Teresa Wagner, DrPH, MS, CPH, RD/LD, CPPS, CHWI, DipACLM, CHWC
References
1Healthy People 2030. Social Determinants of Health. https://health.gov/healthypeople/objectives-and-data/social-determinants-health
2Walker, Renee E., Jason Block, and Ichiro Kawachi. (2012). Do Residents Of Food Deserts Express Different Food Buying Preferences Compared To Residents Of Food Oases? A Mixed-Methods Analysis. International Journal Of Behavioral Nutrition & Physical Activity, 9(1), 41-53.
3Gundersen, C. & Ziliak, J.P. (2015). Food Security and Health Disparities in Children. Health Affairs, 34(11), 1830–1839.
4Healthy People 2030. Leading Health Indicators.
https://health.gov/healthypeople/objectives-and-data/leading-health-indicators
5Abrams, E. & Szefler, S. (2020). COVID-19 and the impact of social determinants of health. https://www.sciencedirect.com/science/article/pii/S2213260020302344